As 2020 turns to 2021, the world seems to be turning the page on this particular time in human history. Anticipation fills the chilly winter air as the world anxiously awaits the end of the era of Zoom calls, masks, air hugs, online-only meetings, and distancing from friends and loved ones. Fueling this optimism has been the deployment of new vaccines for coronavirus, shown to be 90-95% effective at inducing viral immunity in large-scale clinical trials. Such high efficacy was surprising and highly encouraging to both the scientific community and the public, and the results have put a little pep back in our step.
However, as we’ve seen plenty of times this year, the effectiveness of any public health intervention is intrinsically tied to the willingness of the public to cooperate. Vaccines are no exception. And the public, understandably, has some concerns about taking a vaccine that was synthesized and tested in record time. Not to mention, the two COVID-19 vaccines currently being deployed by the FDA are a never-before-seen type of vaccine! All of this has led to some mild hesitation and animosity regarding the widespread administration of the vaccine to citizens.
Here, I’ll try to dispel some of that fear by answering the most pertinent questions about the COVID-19 vaccine and the science behind it. It is my hope that, through this post, you can come to your own decision about the vaccine through an understanding of the facts and data instead of through fear or blind faith. I’ll cover the development process and go in-depth on the actual scientific results reported by Pfizer and BioNTech, the companies that developed the first of the two vaccines. Finally, I’ll discuss why I am confident that these vaccines are humanity’s best weapon against the coronavirus, and why it’s important that everyone embraces the initiative and gets vaccinated as soon as they can.

Table of Contents
mRNA: The Key Ingredient
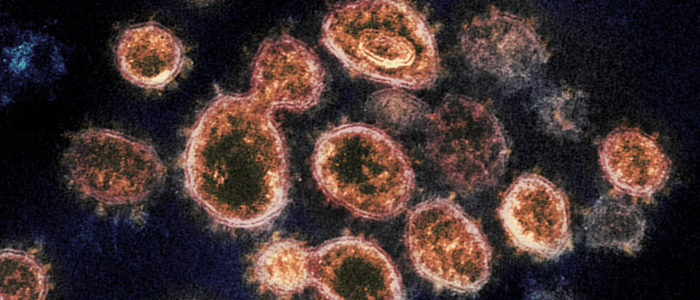
The impact of COVID-19 has led to significant investment and scientific attention to the development of a SARS-CoV-2 vaccine. Although small molecule drugs, like ivermectin and hydroxychloroquine, could potentially mitigate the symptoms of COVID-19, no small molecule drug has ever been able to “cure” a virus scourge. Vaccines, on the other hand, have relegated some highly potent plagues to history’s dust bin. Thanks to vaccines, my generation never had to worry about smallpox, polio, measles, tetanus, and other historically terrifying maladies.
Suffice to say, vaccines are humanity’s best weapon against deadly diseases. They’ve been in use for a long time – ever since Edward Jenner used cowpox pustules to inoculate people against smallpox. For much of the last few centuries, vaccines were administered in the form of dead or inactivated components of the disease, which typically induced a much weaker form of sickness. However, the two coronavirus vaccines developed thus far are a new, different form of vaccines, called mRNA vaccines.

Although mRNA is a newer vaccine technology, there is nothing new about it from a scientific perspective. mRNA, or messenger ribonucleic acid, was first discovered 60 years ago and is commonly taught alongside DNA in 5th grade science classes as an example of a “nucleic acid”, a biologically important type of macromolecule. Its role in human cells is to communicate genetic information from DNA to ribosomes, which convert the mRNA strand into a protein with structure encoded by the RNA strand’s sequence. mRNA vaccines typically encode a specific protein that is essential to the functioning of the targeted disease [1-3].
In the case of COVID-19, currently employed mRNA vaccines target the “spike protein,” which binds to receptors on the cell membrane and allows COVID viruses to latch onto and fuse with cells. Scientists believed this target would be effective because data from other coronaviruses (such as SARS-CoV-1) demonstrated that antibodies to this protein prevented viral infection [4]. Once cells finish making the spike protein, it becomes integrated into the cell membrane and is recognized by a helper T-cell by the process of clonal expansion. “Memory cells” are then created, which learn to remove the spike protein if it ever appears in the body again (for a review on clonal expansion, check out this vaccine post from a while back)!

Since mRNA is downstream from DNA in the flow of genetic information, mRNA vaccines produce immunological resistance without altering the genetic code. This reduces the risk of long-term side effects. Furthermore, the lack of dead or inactivated virus in the vaccine alleviates some safety concerns. Hence, mRNA vaccines represent a safer and more readily deployable virus technology for the 21st century [3].
The downside to mRNA as a vaccine platform, historically, has been a weaker immune response compared to live or attenuated virus vaccines. Part of the reason for this is low cellular uptake. Nucleic acids like mRNA are polyanionic macromolecules, meaning they typically have a strong negative charge. The phospholipid bilayer that separates the interior of cells from surrounding fluid contain loads of fat-bearing “hydrophobic” tails, which strongly deter water, polar, and charged molecules from traveling into the cell. Hence, the cellular uptake and stability of mRNA vaccine carriers has been potentially the biggest hurdle to their deployment as the new vaccine platform of choice. When faced with the challenge of developing a COVID-19 vaccine in record time, the teams at both Pfizer and Moderna knew that they would have to find a way to traverse this obstacle.

Designing the Vaccine
Luckily, Pfizer and Moderna are both good at this sort of thing. To overcome the well-known obstacle of cellular uptake and make a working coronavirus mRNA vaccine, both Pfizer and Moderna settled on an experimental technology used to deliver payloads inside of cells in nanomedicine: lipid nanoparticles. Lipid nanoparticles, or LNPs, encapsulate targets within a fat-loving, or lipophilic, shell. A few different types of LNPs are employed, the most common of which are micelles (where the interior and exterior of the nanoparticle possess different properties) and spherical bilayers (where the nanoparticle is arranged in an ABA sandwich-like format, and the interior and exterior of the NP are chemically similar).

The big advantage to LNPs is that they allow scientists to engineer both the interior and exterior environment of the vaccine. The interior environment, experienced by the mRNA vector, must be chemically polar enough to allow the mRNA molecule to remain stable. The exterior environment, experienced by the solvent and the cell membrane, must be lipophilic enough to traverse the membrane and be uptaken by the cell. In this way, the LNP is almost like a “trojan horse”: it tricks the cell into letting the polyanionic mRNA molecule through. Once across the membrane, the shell is eaten away by fat-digesting enzymes and the mRNA is released. Although this explanation provides a very surface level understanding of the membrane dynamics involved, the engineering of interior and exterior environments of LNPs is a foundational strategy for making tailor-made nano-delivery mechanisms for mRNA payloads. In simpler terms: LNPs are ideal for getting mRNA across the cell membrane, allowing us to conquer one of mRNA’s greatest shortcomings as a vaccine candidate [5].
All told, the final vaccine formulation contains three things: an mRNA strand encoding for the spike protein, a mix of lipids used to form lipid nanoparticles, and salts. The mRNA strand contains two “point mutations” that change certain amino acids in the protein to control how it folds and lock it into a favorable conformation for recognition by the immune system. The salts act as buffers that make sure the vaccine solution doesn’t get too acidic or basic [4]. Notably, neither vaccine contains thiomersal (which was controversial about 15 years ago) or any other preservatives.

Road to deployment
As cool as the vaccine design is, the actual engineering involved took mere weeks after the coronavirus genome sequence was published in early February of 2020. The rest of the long road to actual vaccine deployment involved testing. In vitro testing was done first. There, the ability of the vaccine to actually produce the spike protein is tested in cultured cells. After that, clinical trials begin using human subjects. Clinical trials in America typically involves three phases:
- Phase 1: Small (<100) groups of people are administered the vaccine to test for early effects and dosage. Immunity is tested by blood tests.
- Phase 2: Hundreds of people with different characteristics (such as age and health history) are administered the vaccine. Early effects are noted.
- Phase 3: Thousands of people are given the vaccine to test if it’s effective against the virus. Immunity is tested by infection rate.
This third phase commonly lasts for >1 year, in large part because it takes a long time to recruit enough people who are exposed to most vaccine targets. A number of factors allowed this timeline to be sped up significantly. First, the widespread nature of COVID everywhere in the world actually sped up vaccine development, since it didn’t take long for many people in the trial to be exposed. Pfizer and BioNTech at first had planned to cease the Phase 3 trial after 32 positive cases had been identified in their participants (a very low number for a vaccine trial). However, while their board was negotiating this number, the positive count rose to above 90! The rapid spread of the virus helped speed the testing process, and we ended up with a more statistically robust sample than had been initially planned.
Second, the lifting of regulatory barriers, the prioritization of vaccine-related work by the FDA, and the MASSIVE amount of funding dumped into vaccine research made it feasible to to overlap all three phases of vaccine testing, significantly speeding up the process. Hence, even though the COVID-19 vaccine was developed in record time, the actual development protocol was not shortened to fit the timeline [6]. The scientific community at large recognized how important the safety of this vaccine would be, and Pfizer and Moderna responded to their concern with great care. As a result, this vaccine meets the same safety standards as every other vaccine on the market.
In this section, I will discuss Pfizer and BioNTech’s clinical trial results and road to deployment, just to give you an idea what kind of work it took to get to this point and why there is so much optimism regarding the vaccine results. Pfizer has published their Phase 3 results in a paper in the New England Journal of Medicine here. Moderna published similar results, which you can find here.

The figure above shows the vaccine neutralization titers (VNTs) induced by the administration of various doses of the Pfizer COVID vaccine in Phase 1 trials. To calculate the VNT number, blood samples from vaccinated patients are drawn and exposed to COVID-19 viruses. VNTs represent the dilution factor at which these blood samples effectively neutralize 50% of such “infections.” The higher the VNT number, the stronger the immune response to the viral antigen is. Results show a dramatic increase in the immune response in VNTs after the second dose is administered (Day 21). Moreover, the levels of immunity induced remain fairly stable up until about 50 days. The persistence of the acquired immunity over time is something that scientists will need to keep an eye on as the trials continue. Based on the rate of decrease in the VNTs, Pfizer currently estimates that the acquired immunity will last about a year. More testing is needed to see if this holds true.

Of course, the vaccine wouldn’t be worth much unless it protected against mutant strains of COVID as well. Pfizer and BioNTech researchers tested 18 common variants of SARS-COV-2 in blood extracted from vaccinated patients. The results show broad-sweeping immunity against the most common receptor binding domain variants, including D614G, the most common strain. As new mutations appear, researchers will need to continue ensuring the efficacy of the vaccine against dominant strains. However, the generalizability of the effect thus far is an encouraging sign.

After these encouraging Phase 1 results, researchers moved on to Phase 2 and 3. Here, the vaccine efficacy was tracked in 38,000 patients in a randomized, blinded, placebo-controlled clinical trial. This time, instead of assessing the antibody response in serum, the incidence rate of COVID infection was compared across the control and experimental groups. The figure above shows the cumulative incidence rate across the 119 day clinical trial period, with the blue line representing the control group and the red line representing the vaccinated group. The incidence rate begins identically, but the infection rate of the experimental group drops off dramatically around day 14 after the first dose. The “90% effectiveness” number you’ve probably heard tossed around comes from the difference between the experimental and control group in this experiment. Such a large gap is indicative of a powerful immunological effect!
One thing that gives me even more confidence: the Moderna trial reported almost the exact same powerful protective effect in their version of the coronavirus vaccine! The figure below shows their results. If you mixed up the colors and names, I would have a very hard time telling you which vaccine was which based on the data reported. The fact that two different companies both came up with strong and safe vaccine candidates gives me a lot of hope that the results are for real and that the vaccines are going to protect the people that choose to get them.

What are the risks?
Although the vaccine is effective, you should keep in mind that taking it is not exactly a pleasant time. About 50% of study participants experienced both headache and fatigue on both the first and second dose. A high number of participants also experienced chills, muscle pain, and joint pain on the second dose of the experimental group.

The good news is that more severe adverse effects to the vaccine were extremely rare. Across the board, the incidence of severe effects was inseparable from the control group, indicating that they were likely not due to the vaccine. There were 18 adverse events characterized as “life-threatening” compared to 19 in the control group. Similarly, there were two deaths in the vaccine group and three in the control group. More people withdrew from the study in the placebo group.
The one negative consequence that showed more prominence in the vaccine group than the control was the incidence of Bell’s Palsy, with four total patients developing the condition. Bell’s Palsy is a temporary condition that induces severe weakening of facial muscles on one side of the body. However, this is not an abnormal number of individuals to develop Bell’s Palsy in the timeframe of the study. Typically, about 30 people per 100,000 develop Bell’s Palsy in the span of a year (0.0025% per month). With ~40,000 people involved in both trials being studied over a period of three months, 4 people developed the condition (0.0033% per month). Hence, the incidence of Bell’s Palsy is likely not due to the administration of the vaccine and is more likely just a statistical anomaly. Despite this, the FDA has noted they will keep tabs on the incidence rate of Bell’s Palsy out of an abundance of caution.
Where do we go from here?
What do these results tell us? More than anything, it tells us that we can beat the coronavirus. As bleak as it now sounds, there was a possibility that attempts at inoculation would fail, and that humanity would struggle and lose many lives to the virus for a long time. Now, it appears that we will be able to largely diminish or even eradicate COVID-19’s presence on this Earth, and we could do it soon.
Obstacles still exist. Both Pfizer and Moderna’s vaccines require storage at very low temperatures, and most run-of-the-mill pharmacies don’t have the kind of cryogenic storage they require. Mutations and immune persistence are long-term markers that we must continue to track. Long-term trials are necessary to see if the acquired immunity persists. Our vigilance in the future will be key to determine whether we can beat COVID just for a short time or kill it once and for all.
But above all else, let’s avoid being our own worst enemy this time around.
The pandemic thus far has highlighted the differences in our philosophies about public health interventions as a society. Some people have lots of faith in “the system,” i.e. the government and scientists, to do right by the public. Generally, people with this sort of faith are more willing to trust in social interventions like vaccines. Others, however, seem to have lost their faith in that system, instead realizing that the only people they can trust to protect their family are themselves. Most of the time, this is because the system has failed them in some way in the past.
But make no mistake: I’m not encouraging blind faith in anything. My goal in this post is to help give people understanding and clarity through facts and data. It is my hope that you can feel good about trusting the coronavirus vaccine through your own understanding. Its existence is the product of both incredible brilliance and herculean effort, and to achieve this feat in such a short time is nothing short of a miracle. The only thing keeping it from saving your neighbors’ lives could be you. So please, I implore you, if you have any doubts: reach out to me, and let me know your concerns. I’ll see if I can answer any questions you might have.
Thanks, as always, for reading! Till next time.
References
- G. J. Nabel. Designing tomorrow’s vaccines. N Engl J Med 2013; 368:551-560 DOI: 10.1056/NEJMra1204186
- J R Mascola and Anthony S. Fauci. Novel vaccine technologies for the 21st century. Nature Reviews Immunology 2019; 20, 87-88.
- Maruggi G, Zhang C, Li J, et al. mRNA as a Transformative Technology for Vaccine Development to Control Infectious Diseases. Mol Ther 2019; 27(4):757-772.
- Pfizer-BioNTech COVID-19 Vaccine (BNT162, PF-07302048) Vaccines and Related Biological Products Advisory Committee Briefing Document. Pfizer-BioNTech. Available at: https://www.fda.gov/media/144246/download
- Sahay G, Alakhova DY, Kabanov AV. Endocytosis of nanomedicines. J Control Release 2010; 145(3):182-195.
- Fact Sheet: Explaining Operation Warp Speed. US Department of Health & Human Services. Available at: https://www.hhs.gov/coronavirus/explaining-operation-warp-speed/index.html#:~:text=Operation%20Warp%20Speed’s%20goal%20is,and%20diagnostics%20(collectively%20known%20as
- Walsh EE, Frenck RW Jr, Falsey AR, et al. Safety and Immunogenicity of Two RNA-Based Covid-19 Vaccine Candidates. N Engl J Med. 2020;[ePub]:doi: 10.1056/NEJMoa2027906.
- Mulligan MJ, Lyke KE, Kitchin N, et al. Phase I/II study of COVID-19 RNA vaccine BNT162b1 in adults. Nature 2020; 586(7830):589-93. [ePub] doi: 10.1038/s41586-020- 2639-4.
- Baum, A. et al. Antibody cocktail to SARS-CoV-2 spike protein prevents rapid mutational escape seen with individual antibodies. Science 369, 1014–1018 (2020).
Polack, F. P. et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N Engl J Med 2020; 383:2603-2615.
L. R. Baden et al. Efficacy of the mRNA-1273 SARS-CoV-2 Vaccine. N Engl J Med 2020.